
By Dr Lisa Aufegger, IGHI Research Associate
Patient engagement has become a key priority in today’s health and care systems. And some have argued it’s essential for the sustainability of the NHS.
Patient engagement (PE), the involvement of patients in their medical process, is not a new concept. It first appeared in the late 80s, when the US Food and Drug Administration brought together patients, government, industry, and academia to identify and remove barriers to successful HIV drug and treatment development. Since then, PE activities have blossomed across clinical and non-clinical areas, and generated meaningful insight into and impact on quality improvement in healthcare service and delivery.
“Patient engagement is the activating of interest, attention, and involvement of people who are seeking or receiving medical care, and providing opportunities for them to influence the environment, culture, services, products, or systems of care they experience.” McCurdy et al., 2013.
Success stories
PE activities can bring a range of opportunities, some of which are shown in the image below. For instance, in relation to disease prevention, diagnosis, and treatment, increased PE has shown to facilitate healthier lifestyles; instil seeking information about health conditions; and thus lead to proactive treatment processes.
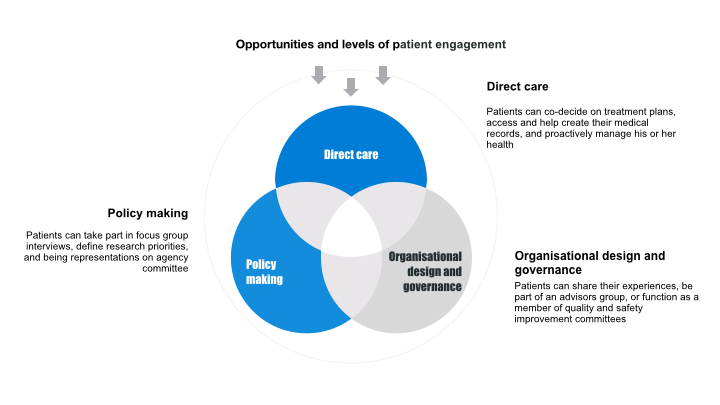
It has also influenced the design and governance of health care institutions. Advocates have been involved in the planning, delivery, and evaluation of better care, creating an active impact on healthcare service and delivery. Last but not least, patients have also participated in policy-making, research and innovation, by shaping research and funding priorities around treatment, device and drug development.
Digital health and patient engagement
Recently, digital health has become a buzzword in facilitating greater PE. Digital health includes integrated, sustainable and patient-centred services, which allow healthcare information storing and sharing, and promote effective communication between patients and healthcare providers. With the introduction of novel digital solutions such as Personal Health Records, patient portals, and mobile applications, PE is aimed to support shared decision-making between patient and healthcare providers.
Interestingly, while the value and potential benefit of these tools are well-recognised, the overall uptake has been relatively low. NHS surveys show that only 12% of patients use online services to, for example, order repeat prescriptions, and less than 3% access their own medical records. In contrast, 92% of patients feel confident in managing their own care, and 40% express the wish to be actively involved in their care. Given such a discrepancy between patients’ desires to be active decision-makers and the low uptake of digital health solutions, what strategies should the NHS use to increase active engagement in patients’ own care?
“Despite the rhetoric and hope for digital health, patients are not using the tools as much as they could.” Birnbaum et al., 2005.
Patient engagement strategies
The success of existing strategies to increase engagement in and uptake of digital health technologies is seemingly varied, and will depend on the characteristics of the patient (such as age, ethnicity); the context (e.g. chronic disease management; patient safety); and the service provider. But as a general rule of thumb, the knowledge, skills, ability, and willingness for a patient to manage their own health care in today’s digital world can be strengthened through:
- Education and training
- Change in culture of health care and delivery
Education and training at a patient level are particularly important to increase (electronic) health literacy. This is the degree to which people have the capacity to obtain, process, and understand basic (electronic) health information and services needed to make decisions regarding their health. There are a range of interventions designed to boost health literacy, from personalised patient information assisted by professional or lay support, to telephone counselling or helplines. These provide patients with the ability to empower themselves, create greater self-efficacy and satisfaction, and ultimately lead to improved health care behaviour and outcomes.
Education and training should also be addressed at staff and organisational level. This will help decrease uncertainty about how to work with patients with limited health literacy, and establish and refine roles, expectations, and new ways of relating to patients.
A change in culture of health care and delivery can be achieved through greater commitment to patient- and family-centred care. But this requires a change in leadership culture and the “doctor knows best” attitude, to allow for patients’ and their families’ active involvement in planning and implementing change.
Patient-and family-centered care has been shown to better support health care and delivery and to enhance patient safety and satisfaction. This is made possible by transforming traditional consulting styles through a collaborative effort to decide care and treatment options between patients, their family and healthcare providers, and by enabling strong communication through health IT innovations.
The future of digital health and patient engagement
Digital health technologies have the potential to enable patient autonomy and proactivity in self-care, which is the ultimate goal of today’s NHS. However, despite patient-engaging care being high on the policy agenda, progress in the NHS has been frustratingly slow. To make change happen, policies and regulations will need to be put in place. These must acknowledge that the future of digital health will not only depend on how well it improves PE, but also how well patients, healthcare providers, and organizations encourage PE at all levels of practice.
“The great promise of digital health is to make it easier and more intuitive for people to manage their health and own their choices. Ultimately, more engaged patients are healthier individuals and that’s the best outcome for all of us,” Tina Freese Decker, COO of Spectrum Health.
Dr Lisa Aufegger is a research associate at IGHI’s Patient Safety Translational Research Centre.