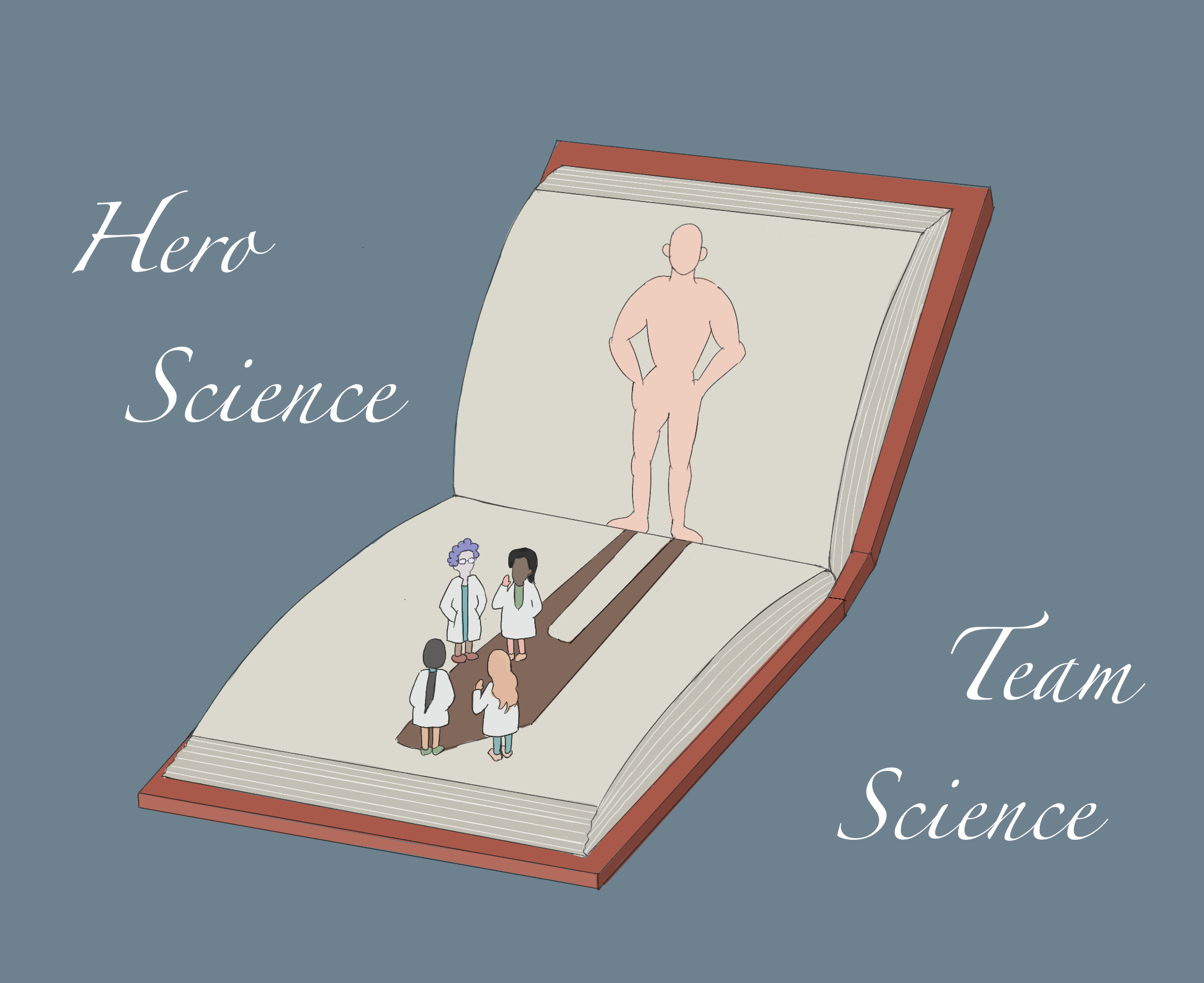
As the leading cause of heart failure in young individuals, dilated cardiomyopathy presents a unique set of challenges and implications. It is an intrinsic heart muscle disease that is the most common reason for needing a heart transplant. The origins of this condition are diverse, spanning genetic predispositions, external triggers that subject the heart to undue stress, or often, a combination of both. Dr Brian Halliday, a Clinical Senior Lecturer and British Heart Foundation Intermediate Fellow at the National Heart and Lung Institute sheds light on this disease and how medical advancements have enabled some patients to go into remission.
Heart failure can be a devastating diagnosis. The prognosis has been shown to be worse than many of the most common cancers. The words themselves often create a sense of doom for patients.
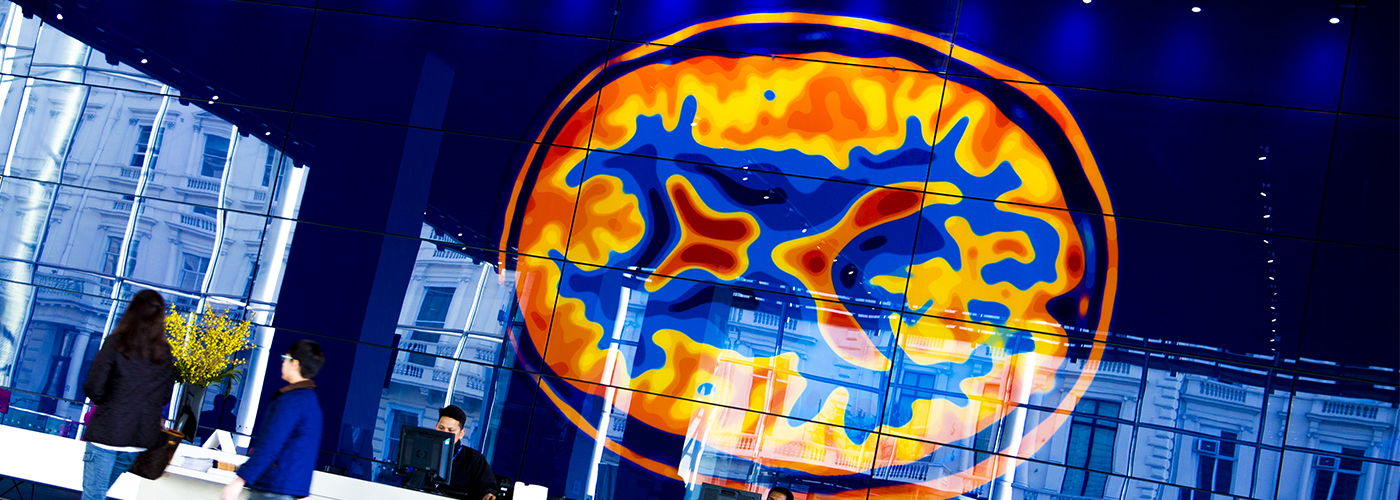
Dilated cardiomyopathy is the most common cause of heart failure in young people and the most common reason to need a heart transplant. It is an intrinsic heart muscle problem where the heart becomes baggy and weak. It may be due to genetic susceptibility, extrinsic acquired triggers that put the heart under stress, or a combination of the two. At the National Heart and Lung Institute, we have a particular interest in dilated cardiomyopathy.