Outline of work
I am a currently Clinical Research Fellow in the second year of my PhD in cardiac regenerative medicine. My PhD is focused on understanding the mechanisms of arrhythmogenesis from stem cell therapy when pluripotent stem cell-derived cardiomyocytes are used to treat cardiac disease and whether the use of biomaterials can mitigate this. Biomaterials hold great promise for the cardiac regenerative medicine field by providing both a platform for both ex-vivo stem cell derived cardiomyocyte maturation and a protective environment for the cells during the immediate / early phase when they are integrating with the host. I am currently investigating how conductive polymers affect ex-vivo myocardial electrophysiology and performing in-vivo engineered heart tissue grafting experiments using a rabbit model of heart failure.
Collaboration
In the last few months I feel that I have been particularly fortunate to benefit from our BHF Regenerative network and our world class collaborators in Scotland and Germany. In the first year of my PhD, I underwent a period of training in complex surgical skills learning the rabbit model from Michael Dunne at Glasgow University in Professor Smith’s lab. I was then able to successfully implement the rabbit model at Imperial College with the help from our excellent CBS staff including Hannah Jones and Philip Rawson and both of our veterinary surgeons Lindsay Benson and Alisdair Gallie. Michael has been instrumental in the success of the model and visited Imperial for the first cases to ensure the implementation was a smooth as possible. We are in the process of developing the percutaneous myocardial infarction model and I look forward to working closely with the team in Glasgow in the future.
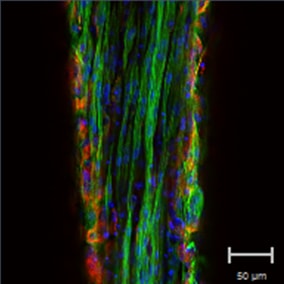
In December, I also visited Professor Eschenhagen’s lab in Hamburg, Germany and worked with Florian Weinberger. It was a very productive trip whereby we have now been able to upscale our engineered heart tissue at Imperial College to a size that is approaching the scale needed for the first-in-human studies. We have now begun our first rabbit grafting experiments at Imperial College. I will be analyzing the arrhythmic burden post grafting and performing ex-vivo optical mapping studies. We are also in the process of characterizing the larger engineered heart tissues. It is an exciting time to be working at the Imperial College BHF Regenerative Medicine Centre! A big thank you to our collaborators and to Thusharika Kodagoda in providing the cells to make the EHTs, and Tom Owen for your continuing help in assisting me with the first grafting experiments!