Maria Piggin from the NIHR Imperial BRC Patient Experience Research Centre shares her experiences of running a co-production training course.
—–
Co-production was first coined in the 1970s by an academic team led by Elinor Ostrom[1] at Indiana University. It stemmed from the lack of recognition of service users in service delivery. There are a number of definitions of co-production; the New Economics Foundation[2] define it as: “delivering public services in an equal and reciprocal relationship between professionals, people using services, their families and their neighbours. Where activities are co-produced in this way, both services and neighbourhoods become far more effective agents of change.”
This concept of equal and reciprocal relationships between different stakeholders to deliver public services is especially important in healthcare. Co-production can give a voice to those with lived experience, helping to define unmet needs, and shape solutions to address those needs.
To date, public involvement (in research at least) has often sought to involve patients and the public after the research question has been identified and sometimes even after the research has already been designed. By comparison, if research is co-produced, relevant patients and/or the public (as well as other stakeholders) would be involved as equals even before the research question had been defined as well as all the way through the project. NIHR INVOLVE has produced helpful guidance on co-producing a research project where it is described as “an approach in which researchers, practitioners and the public work together, sharing power and responsibility from the start to the end of the project, including the generation of knowledge.”

CRISH
Co-CReating Innovative Solutions for Healthcare (CRISH) is one of the UK’s first co-production courses. A two-day short course funded by EIT Health, the course has been delivered twice in London, Barcelona and Grenoble as part of a collaborative project with partners including: Hospital Clínic de Barcelona; ISGlobal; IESE Business School; IrisiCaixa; University of Grenoble; and the Agency for Health Quality and Assessment of Catalonia.
CRISH aims to teach transdisciplinary stakeholders to work together to solve a healthcare challenge by co-creating a project plan for a research project, provision of a service or development of a device/policy or intervention.
We subsequently ran a version of this course at Transform MedEd Conference 2018, which explored the transformation of medical education through innovation and new technologies. The conference is jointly hosted by the Lee Kong Chian School of Medicine, Nanyang Technological University Singapore and the School of Medicine, Imperial College London and brings together educators, researchers, and students from across the world. As the 2018 was attended primarily by medical educators, we adapted the workshop to address co-creation in undergraduate medical teaching. Another Transform MedEd Conference is planned for 2020 and will be hosted by Imperial College in London.
How to run a co-production training course in your setting
Step 1: Who should attend: Groups should comprise stakeholders with varied profiles so that they can learn how to work together. If participants do not attend as an already formulated team, it is essential to commit time beforehand to ensure the groups have mixed stakeholder profiles (preferably with knowledge and/or experience of a common topic e.g. diabetes). Each group should include at least one patient/carer/service user.
Step 2: Breaking the ice: An ice-breaker is an obvious way to get people warmed up and to help people to build new relationships. Our CRISH course starts with an ice-breaker where each team competes to create the tallest tower in 15 minutes using spaghetti, tape, string and a marshmallow. This activity allows all team members (none with an architecture or engineering background!) to use their varied knowledge and skills to build successive prototypes of a tower based on learnings from the previous version and then reflect on this process. These are valuable lessons for co-production.

The teams busy creating their ‘leaning towers of co-production’
Step 3: Choosing a project
Usually the project topic is based on a topic of which the group (particularly the patient/carer/service user) has knowledge and/or experience.. At our workshop, we provided a choice of four public health challenges to solve using curriculum innovation in undergraduate medical teaching. One of these public health challenges was “healthy living in relation to Type 2 diabetes”.
Each group had a facilitator to answer questions and keep an eye on time. Group members were encouraged to think of their own individual ideas on how to address their chosen challenge before the group prioritised one idea to take forward.
Step 4: Mapping stakeholders and assessing their needs.
A stakeholder map is a common tool used in programme management and public health interventions to understand the key actors in a project, where they come from, and their ‘power’ and ‘interests’.
Once identified, stakeholders can be classified according to their level of support and influence in the project; for example, are they ‘Friends’ i.e. those with whom you should maintain communication and employ as ambassadors? Or are they ‘Onlookers’, ‘Champions’ or ‘Blockers’? Classifying stakeholders will mean the relevant engagement strategies can be designed for each.
Once the relevant stakeholders have been identified, their needs can be explored so the project can then be designed to address these. In healthcare, patients, carers and service users are central to identification of t their needs.. A limitation of co-production in a limited time period was that groups often had to hypothesizethe needs of the relevant stakeholders where they did not have the stakeholder reprsentatives present. Students are a vital stakeholder in the design of undergraduate medical curriculum, and we were lucky to have at least one medical student in each team at our conference workshop.
Step 5: Designing and evaluating the project
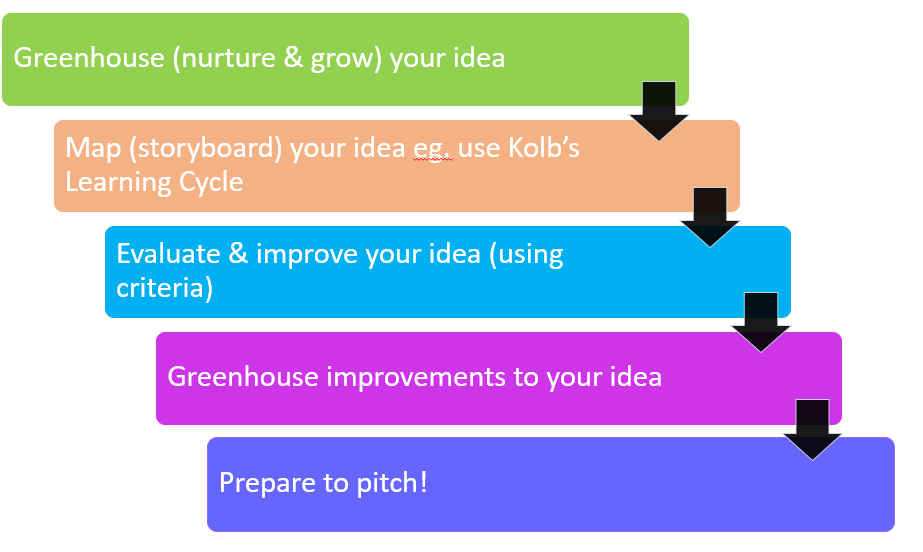
The design stage involves each group ‘greenhousing’ (nurturing and growing) their idea/project (or in our conference workshop, their curriculum innovation) and is supported by each group’s facilitator. This stage may involve further discussion, research, mapping or prototyping using various creative materials; for example, storyboarding a care pathway. In our training course we provided copies of Kolb’s Learning Cycle to which teams could refer..

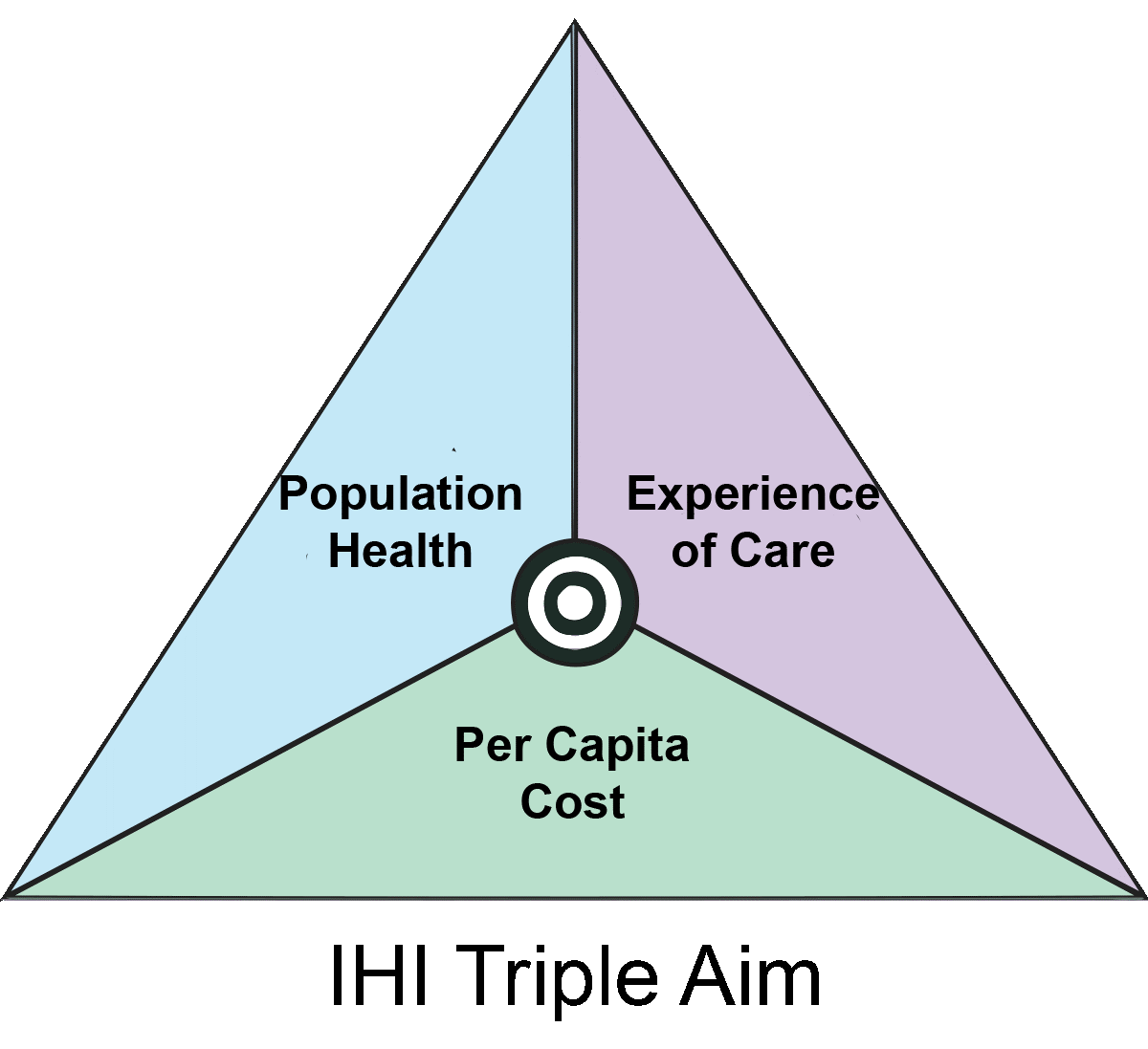
A key part of the design process is evaluating the project plan to further improve It, so providing teams with some evaluation criteria is useful. In our CRISH course one of the criteria was whether the project plan addressed the Institute for Healthcare Improvement (IHI)’s ‘Triple Aim’:
- Improving the patient experience of care (including quality and satisfaction)
- Improving the health of populations; and
- Reducing the per capita cost of healthcare
In our conference workshop, participants were provided the following evaluation criteria:
- Are stakeholder needs met?
- Does the proposal have the ability to address the challenge?
- How novel is the idea?
- What is the speed to implementation?
- What is the ease of implementation?
- What is the cost of implementation?
Once each group evaluated their project design against these criteria, they were encouraged to further ‘greenhouse’ improvements to the project plan.
Step 6: Pitching of Ideas/Project Plans
Finally, teams are asked to pitch their project plans either as a group or by nominating one member to do so. In the CRISH course, we provided a short training session on how best to deliver a pitch including having a “wow” moment. It was great to see so many student team members present their group’s pitches at the conference.
Some reflections and the future for CRISH.
Co-production is not something which can be achieved in a workshop (or even over a 2-day course). Co-production requires careful planning, a commitment to identifying and involving all relevant stakeholders, sharing power and responsibility, time to form relationships and reflection.
If groups attend co-production workshops with an existing challenge and are keen to problem solve, they can hopefully use the plan created in the workshop (and perhaps even involve some of their group as stakeholders) in making it happen in their local context, as was the case for the MatImms project.
Even though getting all the relevant stakeholders together at the same time may be challenging, co-production workshops provide a unique opportunity for groups of different stakeholder profiles interested in addressing a challenge to have time and space to work together away from the pressure of their everyday roles.
Our conference workshop had some obvious limitations including not having all relevant stakeholders represented in each group (especially patients/carers/service users) and the limited time in which groups had to design their curriculum modules as the whole workshop was only 1.5 hours. However, some great ideas were developed in a short time which is promising for projects not limited to 1.5 hours! One proposal for the “healthy living in relation to Type 2 diabetes” challenge was that the students be divided into teams and each team would be mentored by a diabetes patient and/or caregiver.
The current CRISH project is developing a ‘train-the-trainer’ framework with new academic partners including Heidelberg, Uppsala, Coimbra and Lodz who will deliver the course in their local contexts. This will enable the future sustainability of the course.
Maria Piggin, NIHR Imperial BRC Patient Experience Research Centre
[1] Ostrom E. Crossing the great divide: coproduction, synergy, and development. World Dev. 1996;24:1073‐1087.
[2] https://neweconomics.org/uploads/files/312ac8ce93a00d5973_3im6i6t0e.pdf (05-Jul-19)
